Morphology
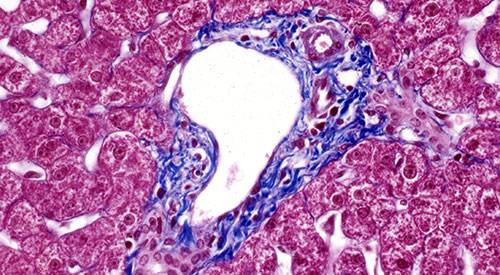
The Cima Morphology Platform is a support service for researchers, both from our center and from other companies, a histology service specialized in the processing of samples.
Specifically, the following techniques are offered:
- Processing of paraffin-embedded tissues: inclusion, cutting and staining.
- Frozen tissue processing: freezing, cutting and staining.
- Immunohistochemical/immunofluorescence techniques: antibody counseling, performance and tuning. Single and multiple labeling.
- Design and elaboration of Tissue Microarrays (TMAs).
- Design of experiments involving histological techniques.

Do you need our services?
If you are interested in knowing our rates and contracting our services, please contact us.
Our platform services
Research Support Unit

Processing of biological samples
Inclusion, cutting and staining of samples in kerosene. Cutting and staining of frozen samples. Immunohistochemistry, immunofluorescence, construction and cutting of TMAs.
Use of equipment
Researchers have at their disposal, upon reservation, the use of our equipment for sample preparation.
Sample extraction procedures
Collect specimens with sharp dissection material. Hold and cut the specimens by the edges and without pressing them, so that the areas of interest are not damaged. Sometimes, it is better to perform the carving once the specimens are partially or completely fixed (depending on their size). The specimens should be introduced into the fixative as soon as possible to avoid autolysis. It is best to fix each specimen (or group of identifiable specimens) in an individual (wide-mouthed) vial of the appropriate size, depending on the volume of fixative required. In most cases, 100 ml urine bottles are adequate.
Fresh tissue tends to stick to each other and to the bottom of the bottle, which makes fixation difficult. Therefore, it is advisable to shake the flasks once or twice to separate the tissues from each other and/or from the bottom of the flasks. If there is enough blood in the fixative after tissue collection, replace it with new fixative. Fixative should not be reused.
- Fixative volume: The ratio of fixative/tissue should be at least 20:1 (vol/vol). If the amount of fixative is not adequate or the specimen is too large or too thick the inside of the specimen will not fix properly. One of the most frequently encountered problems is insufficient fixation. When samples are large, it is advisable to open them in half or to make several smaller fragments (maximum thickness 3-4 mm). The red-pink color of fresh tissues changes to brown with fixation. The presence of a red-pinkish hue anywhere on the specimen (including inside) is a sign of insufficient fixation.
- Fixation time: For specimens with a thickness of about 3-4 mm, a fixation time of 24-48 h is sufficient. In thicker specimens, it is common to observe that the periphery of the specimen is fixed, but not the center of the specimen. Therefore, in these cases, it is advisable to make fragments with a maximum thickness of 3-4 mm so that the fixation is adequate.
Once the fixation is finished, the fixative is removed, the samples are washed with running water to remove the fixative residues and then transferred to 70% ethanol. The samples are then placed in properly identified cassettes, previously carving them, if necessary.
Once the cassettes are in 70% ethanol, it is convenient to transfer the samples to the Service as soon as possible to proceed to their inclusion in kerosene. The tissues can remain in 70% ethanol for a few days, but not too long, since the samples dehydrate and harden due to the action of ethanol, which makes it difficult to obtain optimal sections later on. Tissue samples are best stored in the form of kerosene blocks. The blocks can be subsequently cut and stained.
For fixation, use flasks of the appropriate size so that the ratio of sample volume to fixative volume is met. In most cases, 50 or 100 ml bottles are sufficient.
Mark the bottles (not the lids, since errors can occur due to interchangeability) with the identification of the sample and cover it with transparent adhesive tape to prevent it from being erased by contact with 70% ethanol. The bottles should be wide-mouthed (e.g. urine bottles) in order to be able to extract the sample easily and without damaging it.
Do not use tubes with conical bottoms, since the samples sink, they can be deformed into the conical shape of the bottom and there is not enough fixative in the vicinity of the sample.
For the cassettes, place them in a wide-mouthed bottle of sufficient volume for the corresponding number of cassettes. Use as many bottles as necessary and identify all of them with adhesive tape indicating the name of the investigator and the laboratory number.
Make sure that there is enough 70% ethanol to cover all the cassettes (relatively often we find that the top cassettes are not covered and the samples dry out).
Do not use recycled culture media bottles as it is difficult to remove the cassettes inside.
Identify the cassettes as indicated below. The identification should be written with a fine hard lead pencil, in clear handwriting and should be unambiguous.
Some of the histology markers or other supposedly solvent-resistant markers are partially erased during the embedding process by the combined action of ethanol, xylol and hot kerosene. If this occurs, the samples cannot be identified.
The cassettes must be identified on the front side. Information on the sides will not be transcribed on the carrier. Samples should be coded, i.e. an identification should be used for each sample that is brief (no more than 6-8 characters), but unambiguous. The experiment should not be described/summarized on the cassette. Small letters are very difficult to read correctly, especially if they are kerosene coated. Pay attention to numbers such as 4 and 9 and letters C and G; D, O and Q; and U and V which are often confusing.
*Illegible identifications are one of the most frequent problems we encounter.
It is very convenient to perform the milling when the specimens have already been fixed. Use sharp blades. Otherwise, or if the carving is performed on fresh (unfixed) tissue, it is very likely that the specimen will be torn and the cutting surface will not be flat. This will make the work of the technical personnel more difficult, more tissue will be lost in the cutting process and the quality of the cuts obtained will be reduced.
The purpose of the carving is twofold, on the one hand it allows a correct dehydration and inclusion in kerosene and, on the other hand, it indicates the orientation that should be given to the piece in the kerosene block to obtain the cuts with the desired orientation. The samples should not be thicker than 3-4 mm (slightly less than the depth of the cassettes). The specimens should clearly distinguish the orientation that the piece should have for the cut. At the time of inclusion, the specimens should rest on the larger surface, which should also be as flat as possible. If another cutting orientation is required, this must be expressly indicated when the specimens are delivered to the Service.
Once the samples have been cut, they are placed in the corresponding previously identified cassette and the latter in a container with 70% ethanol. Take the samples to the Service shortly to proceed to their inclusion in kerosene.
If there is an area of particular interest in the sample, e.g. a tumor, carve the tissue so that the area of interest is close to one surface of the sample and place it face down in the cassette. If the area of interest is small, inform the personnel of the Service so that it is not lost. Keep in mind that it is very difficult to carve and include the sample so precisely that it is difficult to know prior to the cutting process which cuts will contain the area of interest. In these cases, it is advisable to request serial slices and collect all the slices until you are sure that you have obtained the necessary information. It is always possible to re-cut a block and obtain deeper slices, but the discarded slices are lost forever.
Do not introduce too many tissues in the same cassette. In the case that several samples are included, the size of the samples should allow them to fit loosely in the cassette and all of them in the base, i.e., never introduce some samples on top of others. As a general rule, place samples of similar consistency in the same cassette. For example, do not introduce together hard tissues, such as skin, and soft tissues, such as spleen or brain, because if the consistency varies too much it will not be possible to cut them all properly. Nor is it advisable to put samples of very different sizes in the same cassette. For example, a mouse lymph node with a liver/kidney/lung sample, etc. By the time an acceptable surface area is obtained from the larger sample the small sample will have disappeared, i.e., it will have been exhausted without having obtained any cut-offs.
If the sample is very small, use biopsy cassettes (smaller hole) to prevent the sample from being lost in processing. Biopsy cassettes should not be used for larger specimens, which are not at risk of coming out of the cassette holes in the kerosene embedding process.
There are many variables that affect the quality of frozen cuts. Several methods may have to be tried until the most suitable one is found. Keep in mind that it may be difficult to obtain acceptable cuts from some tissues. Fatty tissues are a good example.
Both fresh and previously fixed tissues can be frozen, depending on the compatibility with the techniques to be applied later on the sections. Fresh tissues should be frozen immediately after extraction. Carve the samples following guidelines similar to those described in the section on paraffin-embedded samples.
In case the tissues are fixed, it is convenient to cryoprotect the samples before freezing. For this purpose, after fixation, the samples are placed in 20% PBS-sucrose and kept at 4°C until the sample sinks in the solution (usually until the following day). Freeze the sample by one of the methods described.
We recommend, if compatible with the specimens, embedding them in OCT using freezing molds (available from the Service). The embedding medium helps remove heat from the specimen during the freezing process, helps protect the tissue from desiccation during storage and supports the tissue in the cutting process.
Use the appropriate mold size for the size of the specimen (it should fit in the bottom of the mold leaving a space around the specimen). Mark the mold (repeat on two sides) with the sample identification using an indelible marker. Follow the same rules described for the identification of the kerosene cassettes.
The volume of OCT needed will depend on the size of the sample, it should cover and exceed about 2 mm of the sample. Pour OCT into the previously identified mold taking care not to form bubbles as they make it very difficult to obtain adequate slices. If there are bubbles, remove them with tweezers. Insert the piece of tissue to the bottom in the desired orientation, avoiding the formation of bubbles.
If the tissue is not fixed, freeze as soon as possible using one of the methods described below. If the tissue is fixed, place the specimen on filter paper to absorb the cryoprotectant solution (PBS-sucrose) from the surface of the specimen. Insert the specimen into the mold with OCT as described above.
A simple method consists of freezing with dry ice (-78ºC) in the form of a pellet in an expanded polystyrene box (polystyrene foam or white cork). This method has advantages for its safety and simplicity and is more useful and convenient when a relatively large number of samples are to be frozen. Insert the cryo-mold with the OCT and the sample into the dry ice so that the OCT surface is horizontal. Wait for it to freeze. Store the frozen samples at -80°C. Under no circumstances should frozen samples be placed in liquid nitrogen (-196°C) as it is very likely that the blocks will crack due to the abrupt temperature change. The cutting process and, therefore, the quality of the cuts will be affected.
The best method is to use isopentane (2-methyl-butane) pre-cooled to its freezing point (-160°C) as freezing is faster than with the previous method. Introduce a Pyrex beaker with isopentane into a Dewar beaker with liquid N2 carefully so that the N2 does not mix with the isopentane. Use long forceps or, better yet, a beaker holder with a handle designed for this use. Remove the beaker when the isopentane starts to freeze (a kind of white lentils appear at the bottom). With the help of forceps, insert the freezing mold with OCT and the correctly oriented sample into the isopentane without immersing it and hold it until it has frozen. Remove the sample from the isopentane and keep it on dry ice. Chill the isopentane again as many times as necessary to freeze all tissue samples.
Muscle is the exception in terms of tissue freezing methods.
It must be frozen using cold isopentane or artifacts will appear due to the formation of ice crystals. Pre-cool the isopentane with liquid N2 as described above and introduce the muscle sample directly into the cold isopentane (do not use OCT).
Store the samples in properly labeled cryotubes.
Frozen samples are stored in a -80°C freezer. Samples must be protected from desiccation, even if they are frozen in inclusion medium (OCT), so that they do not spoil.
Each sample can be well wrapped in aluminum foil (best double-layered), noting the identification of the sample on the foil with an indelible marker (before wrapping the sample) to facilitate later location. This step is not necessary if the samples are to be cut immediately afterwards.
Put the samples in boxes (suitable for -80ºC) properly identified and store them in the freezer. In any case, it is best to cut and stain the cuttings as soon as possible. Frozen samples well protected from desiccation can be stored for up to 2-3 years at -80ºC. If the samples are dried out, the OCT takes on a plastic-like appearance and it is almost impossible to cut the samples.
Sample delivery instructions
*At the time of delivery of the samples to the SM, the corresponding completed request form must be attached.
- Samples for kerosene embedding: Samples must be already fixed, carved and in properly identified cassettes. The cassettes should be delivered inside a closed vial completely covered with 70% ethanol. Identify the vials with the name of the investigator and laboratory number on an adhesive tape.
- Frozen: samples should be delivered properly frozen and transported to the MS on dry ice. It is advisable to contact the Service staff (x5022) beforehand by telephone to ensure receipt of the samples.
It is advisable to attach a list of the samples delivered and indicate any special instructions. If samples are delivered without instructions, they will be included, cut and stained following standard protocols. Indicate any special requirements each time samples are submitted.
In the Morphology platform we keep a record of all requests, but many times months go by since the last similar request and sometimes it is difficult to know if we are taking the correct one as a reference.
Meet the research team




